COX inhibitors alleviate chronic pain. These medications are anti-inflammatory. COX inhibitors are useful in treating numerous pain syndromes in many disorders. This activity examines their indications, actions, and contraindications. This activity will highlight the mechanism of action, adverse event profile, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant interactions) relevant to multi-disciplinary health team members managing chronic pain syndromes and related conditions.
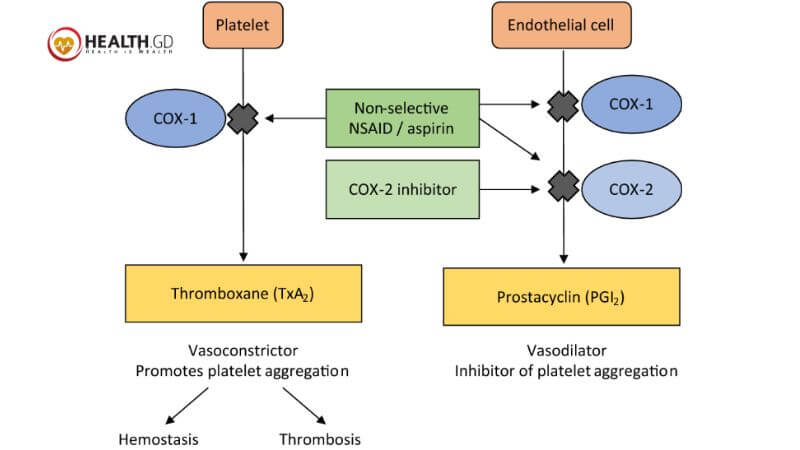
COX-2 inhibitors relieve pain and inflammation differently than NSAIDs. Moreover, COX-1 and COX-2 are the primary COX enzymes. Both kinds create prostaglandins, but COX-1 enzymes produce baseline levels that activate platelets and protect the gastrointestinal tract, whereas COX-2 enzymes release them following infection or damage.
COX-2 Inhibitors are NSAIDs
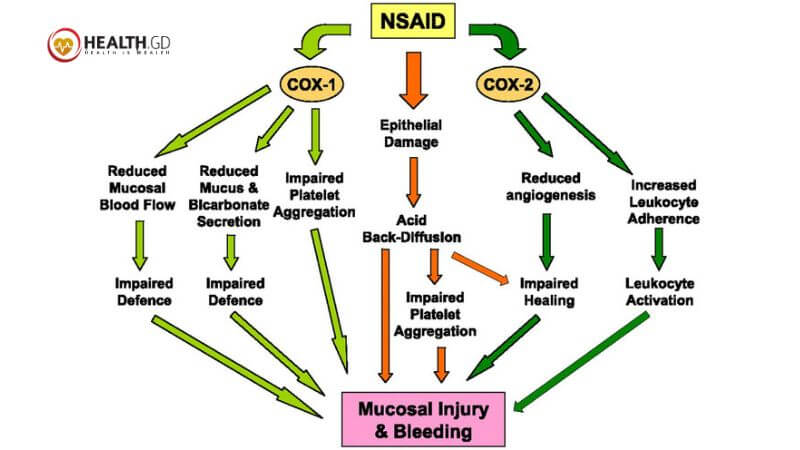
COX-2 inhibitors are NSAIDs that block COX-2 enzymes. NSAIDs diminish inflammation, discomfort, and fever. Although COX-1 inhibitors (blockers) prevent inflammation, they also impede stomach and intestinal lining protection and blood clotting control. COX-2 enzymes produce pro-inflammatory prostaglandins. Most COX-2 inhibitors reduce inflammation.
COX-2 drugs relieve inflammation and pain with fewer gastrointestinal side effects than NSAIDs that inhibit both COX-1 and COX-2 enzymes. They have gastrointestinal side effects, and like other NSAIDs, they increase stroke and heart attack risk.
Action Mechanism
COX inhibitors include aspirin, c2s NSAIDs, and non-selective NSAIDs. NSAIDs include ibuprofen, naproxen, ketorolac, and indomethacin. C2s NSAIDs exclusively have celecoxib. Meloxicam and diclofenac are unclassified cox-inhibitors. The cox enzyme converts arachidonic acid to prostaglandin. It contains two isoforms, COX-1 and COX-2. Each of the roughly 20 COX inhibitors inhibits each isoform differently. Moreover, COX-1 controls platelet aggregation, kidney afferent arteriole vasodilation, and stomach mucosa acid protection.
COX-2 inhibition is predominant in C2s NSAIDs. Although aspirin suppresses COX-1 more than COX-2, it does so permanently.
Administration
Oral COX inhibitors are the most frequent. You can take ketorolac intramuscularly or intravenously. Topically applied COX inhibitors exist. Topical NSAIDs have the fewest systemic negative effects.
How Do COX Inhibitors Work?
As you know, your body has two COX enzymes, COX-1 and COX-2. Both enzymes produce prostaglandins. The hormone-like prostaglandins promote inflammation, discomfort, and fever. The sole enzyme that generates prostaglandins, which help your blood clot and protect your stomach and intestinal lining from digesting acids, is COX-1.
Although COX-1 inhibitors (blockers) prevent inflammation, they also impede stomach and intestinal lining protection and blood clotting control. COX-2 enzymes produce pro-inflammatory prostaglandins. Most COX-2 inhibitors reduce inflammation. COX-2 inhibitors do not suppress COX-1. This preserves your stomach and intestinal lining and blood clotting.
COX Inhibitors Are Widespread Drugs
Although over-the-counter, they can cause significant negative effects including death. Patients should consult their doctors before using COX inhibitors, especially for a long time. Clinicians should advise patients to carry a list of drugs, including OTCs, at all times. Risky patients may need renal function monitoring and endoscopy. Renal function and coagulation monitoring use level III evidence.
Aspirin-taking patient requires consultation with the prescribing doctor.
All interprofessional healthcare team members must be informed of NSAID contraindications and side effects when a patient has a GI bleed. Gastroenterologists, primary care doctors, nurses, and chemists must communicate well. The patient’s documentation and communication should explicitly state the contraindication. Since nurses have more regular contact with patients, they can assess therapy efficacy and monitor side effects. The chemist can check the dose, and medication interactions, and inform the physician. All interprofessional team members must communicate and coordinate for COX inhibitor therapy to optimise patient outcomes.
When Do COX-2 inhibitors work?
A dosage relieves pain within 60 minutes. COX-2 inhibitors’ anti-inflammatory actions require days to take effect. Short-term pain treatment (days to weeks) requires the lowest dose for the shortest duration.
For arthritic pain treatment, your doctor will analyse your health history and lab testing to decide if this medicine is safe to use regularly. Your doctor will evaluate your health history and blood testing to see if this medicine is safe. Importantly, always follow your doctor’s or medication’s dose instructions. Call your provider with questions.
What are COX-2 inhibitor risks?
COX-2 inhibitors may raise complications like Strokes and heart attacks. COX-2 inhibitors raise risk in all users, especially those at risk for heart disease and stroke. These dangers may increase with higher doses or prolonged usage.
Gastrointestinal issues. Stomach and intestinal perforation, ulcers, and bleeding can be fatal. Any time, without symptoms, these responses might occur.
Are COX-2 Inhibitors Safe?
COX-2 inhibitors increase fatal heart attack and stroke risk. The risk rises with dose and treatment duration. People with specific cardiac issues, stroke history, or heart bypass surgery should not use Celebrex.
People with active GI ulceration, bleeding, or inflammatory bowel disease should use celecoxib with care despite its decreased risk of GI side effects. Life-threatening GI side effects including stomach or intestinal bleeding are more common in the elderly and those using stomach-irritating medications.
COX-2 inhibitors may delay blood clotting, increasing haemorrhage risk. Children under two cannot use COX-2 inhibitors. Doctors should advise against using most NSAIDs, including celecoxib, during the last three months of pregnancy or nursing. Please see the celecoxib medication monograph for a comprehensive list of adverse effects.
What Are COX-2 Inhibitor Side Effects?
Long-term usage of COX-2 medications at higher doses increases adverse effects. Bloating, diarrhoea, constipation, stomach lining irritation, nausea, and vomiting are gastrointestinal side effects. Some COX-2 inhibitors cause headaches and dizziness.
However, COX-2 inhibitors may slow renal blood flow. They can induce salt and water retention, edoema, and excessive potassium. They can sometimes affect the kidneys more severely.
COX-2 inhibitors increase heart attack and stroke risk. Heart-related adverse effects include high blood pressure, congestive heart failure, and palpitations. Please see the celecoxib medication monograph for a comprehensive list of adverse effects.
Therefore, after the discontinuation of rofecoxib in 2004 and valdecoxib in 2005 due to increased heart attack and stroke risk, celecoxib is the sole COX-2 inhibitor in the U.S. Although generic, celecoxib is more costly than nonselective NSAIDs. Celecoxib reduces pain and inflammation as well as NSAIDs like ibuprofen, diclofenac, and naproxen, but it has fewer gastrointestinal side effects. It increases cardiovascular event risk like nonselective NSAIDs. Celecoxib somewhat reduces COX-1 enzymes at higher doses.
COX-2 inhibitors treat:
- Spondylitis
- Juvenile RA
- Primary dysmenorrhea
- Sports injuries cause acute agony.
- Osteoarthritis
- Rheumatic arthritis
Which COX-2 Inhibitors Are Available?
The sole COX-2 inhibitor is Celecoxib (Celebrex) and the generic version is available in the US. Moreover, long-term use of rofecoxib (Vioxx) and valdecoxib (Bextra) raised the risk of heart attacks and strokes, therefore they were recalled in 2004 and 2005. Nonsteroidal anti-inflammatory medications (NSAIDs) decrease inflammation but are distinct from steroids. For joint inflammation (arthritis) and other tissues including tendinitis and bursitis, NSAIDs decrease pain, fever, and edoema.
These medications include aspirin, indomethacin (Indocin), ibuprofen (Advil, Motrin), naproxen (Naprosyn), piroxicam (Feldene), and naprodetone (Relafen
Millions take NSAIDs to manage inflammatory pain, fever, and edoema, as well as pain alone. NSAIDs inhibit prostaglandins, which cause inflammation-related discomfort and edoema.
Conclusion
To conclude, COX inhibitors are anti-inflammatory medications used to alleviate chronic pain and treat various pain syndromes. Also, COX-2 inhibitors block COX-2 enzymes, reducing inflammation and pain with less gastrointestinal side effects. They also have gastrointestinal side effects and increase the risk of stroke and heart attack. COX enzyme converts arachidonic acid to prostaglandin, producing pro-inflammatory prostaglandins. Most NSAIDs affect both COX-1 and COX-2 enzymes, making them nonselective.
COX-2 drugs target COX-2 enzymes more accurately. Lastly, Patients should consult their doctors before using them and carry a list of drugs at all times. Interprofessional healthcare team members must be informed of NSAID contraindications and side effects, including gastrointestinal bleeding, to optimize patient outcomes.








